| |
The Reverdin-lsham Procedure for the Correction of Hallux Abducto Valgus |
Preoperative Criteria |
|
This procedure is directed at the structural correction of the deformities of HAV that are manifested at the metatarsal head. Specific criteria for the Reverdin-Isham procedure are:
- A symptomatic medial bunion deformity
- A good range of motion of the first MPJ; no pain, no crepitus, and no degenerative changes
- A congruous or deviated joint
- An intermetatarsal angle of 20° or less for rectus foot and 16° or less for an adducted foot
- An increased PASA
- A normal DASA
- HA angle measurements that are from slightly to highly abnormal
- A hallux axial rotation that is mild or absent
- Relative metatarsal protrusion that is normal to positive
If the DASA is abnormal, then the Reverdin-Isham procedure should be combined with an Akin procedure. A plantarflexed first metatarsal may or may not be present. Another procedure to correct a plantarflexed metatarsal is not needed.
|
| |
Operative Techniques |
|
The Reverdin-Isham procedure is performed using one of two surgical techniques: a minimal incision technique, and an open exposure technique.
Minimal Incision Technique |
|
A 1.5-cm longitudinal incision is made on the planter medial aspect of the first metatarsal head. The incision is carried deep through subcutaneous tissue to expose the capsule of the first MPJ. A capsulotomy is performed, and the dorsal medial aspect of the head is freed of the capsule and ligaments attachments. The medial eminence is then resected. The dorsal eminence and the tibial sesamoid is palpated and identified through the skin. A bone cutting instrument (e. g., Shannon 44, United American Medical, McMinnville, Tennessee) is inserted into the incision, and an angular medial wedge osteotomy is performed from dorsal distal to planter proximal in the metaphyseal portion of the head of the first metatarsal. Care must be taken to preserve the lateral cortex and the articular surface of the halluxal sesamoids and the dorsal articular surface of the head. The LIXIscope (Lixi Inc., Downers Grove, Illinois) facilitates placement of the osteotomy and indicates the amount of bone to be removed. The hallux is then rotated into adductus, and the osteotomy is compressed and closed. Remaining osseous structures are rasped smooth.
Attention is then directed to the lateral aspect of the first MPJ where a 0.5-cm oblique incision is made over the first MPJ. The incision is deepened, and a lateral capsulotomy and an adducto hallucis tenotomy is performed. Skin edges are approximated using 4-0 nonabsorbable suture. If indicated by an increased distal articular set angle, an Akin procedure is performed. I have found that an Akin procedure is indicated in most cases. The wound is dressed, and position is maintained with a sterile splint dressing of the surgeon's choice.
Postoperative Management
The patient is given a wooden postoperative shoe and discharged. The patient is allowed to increase ambulation to tolerance. Postoperative pain, as with most ambulatory procedures, may require minimal amounts of pain control medication. Many patients take none.
The dressing is changed on day 2 or 3 after surgery, and the sutures are removed. A splint dressing is reapplied. The second dressing change occurs 1 week after surgery, and a removable splint dressing is applied and changed daily by the patient. Bathing is permitted. The patient is allowed to ambulate in a self surgical shoe or a supportive athletic-type shoe until normal shoes can be worn. Postoperative radiographs are taken on the first redressing and again 3 to 4 weeks after surgery for evaluation of healing. It should be noted that, as with an Austin-type bunionectomy, a minimal amount of bony callous formation is expected.
|
| |
Open Exposure Technique |
|
A 6.0-cm longitudinal incision is made over the dorsal aspect of the first MPJ medial to the extensor hallucis longus tendon. The incision is deepened through the subcutaneous tissue, exposing the joint capsule. A capsulotomy of the surgeon's choice is performed, and the head is freed of the capsular and ligamentous attachments. The head of the first metatarsal is delivered through the incision, and the medial eminence is then resected. A lateral capsulotomy and adductor hallucis tenotomy are performed.
Attention is then directed to the first metatarsal head, where an angular medial wedge osteotomy is performed using a bone cutting instrument of the surgeon's choice. The angulation is from dorsal distal, at the termination of the cartilage on the dorsum of the head planter proximal, to the termination of the cartilage on the planter surface of the metatarsal, posterior to the sesamoids. The lateral cortex is left intact. The osteotomy site is closed, correcting the structural deformity on two planes. Internal fixation is the prerogative of the surgeon. The capsule is closed using 3-0 absorbable sutures; skin is sutured with 4-0 subouticular closure. If it is indicated by an increased distal articular set angle, an Akin procedure is performed. The wound is dressed with a sterile splint dressing of the surgeon's choice.
Postoperative Management
Postoperative care for the open techniques is the same as for the minimal incision technique with one exception. The foot is kept in the wooden postoperative shoe for 3 to 4 weeks. It is my opinion that the open technique requires more soft-tissue dissecting, resulting in increased instability at the osteotomy site. This increased instability indicates longer use of the wooden postoperative shoe.
|
|
| |
Postoperative Bandaging |
|
Minimal incision procedures, by design, are very traumatic, with a minimal amount of soft-tissue disruption. A second metatarsal, for example, has seven tendons passing over the MPJ. These tendons pass over the dorsal, medial, planter, and lateral aspects of the MPJ. The head of the second metatarsal is also stabilized by a strong intermetatarsal ligament, attached to the third, fourth, and fifth metatarsals. A properly performed osteotomy at the proximal aspect of the metatarsal head does not disrupt these soft-tissue structures. These structures, during the initial postoperative healing phase of the first 3 to 6 weeks, contract and stabilize the osteotomy site. This contracture of the soft-tissue structures is called "intrinsic fixation." Although internal fixation is not required, external splinting is required to enable the patient to bear weight.
Postoperative splint dressings in minimal incision foot surgery should stabilize the surgical site in its corrected position, be a comfort to the patient that is easy to apply, and maintain a sterile barrier.
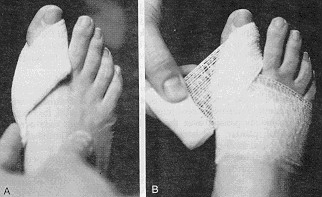
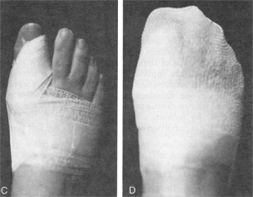
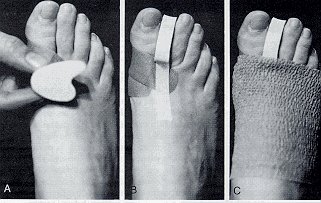
My postoperative dressings are presented in two phases. The first phase represents the type of dressing used during the first postoperative week. These dressings are applied by the surgeon. The second phase of dressings are those splint dressings used for the following 4 weeks. Figure 8 represents phase one dressings, and Figure 9 represents phase two dressings. The phase two dressings are initially applied by the surgeon and are changed daily by patients after they have been instructed in their application. Bathing is permitted on a daily basis after the first postoperative week.
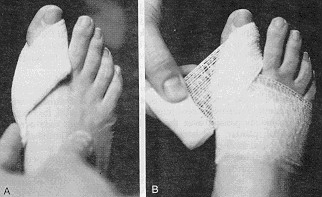
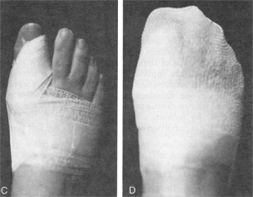
Figure 8
Bandaging techniques.
- Placement of a 3 inch X 3 inch gauze pad adducting the hallux.
- Maintaining placement of the gauze pad with the application of 2-inch Kling (Johnson & Johnson, New Brunswick, New Jersey) wrap.
- Dermacil (Johnson & Johnson, New Brunswick, New Jersey) tape splints the hallux in the corrected position.
- The final dressing.
 |
|
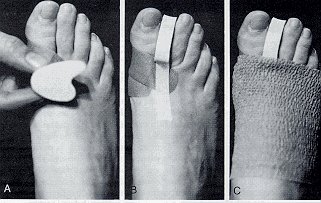
Figure 9
The second phase of dressing is applied 1 to 4 weeks after surgery.
- A large toe separator is placed between the first and second digits.
- The separator is taped in the appropriate position.
- Coban elastic wrap (3M Co., St. Paul, Minnesota) stabilizes the forefoot.
|
|
|
|
|