| |
Protocol of Treatment of Hallux Valgus in Minimal Incision Surgery
By Dr. Roque Esteban Galaz Lopez, MD
Orthopedics and Traumatology
President of the Mexican Association of Ambulatory Foot and Ankle Surgery
Associate Professor of The Academy of Ambulatory Foot and Ankle Surgery
Av. Tamaulipas 601
Tampico Tarns Mexico
Adaptation and translation by:
Translated by Stephen Isham, MD
Member of the Mexican Association of Ambulatory Foot and Ankle Surgery
International Director and Professor of The Academy of Ambulatory Foot and Ankle Surgery
|
| |
Introduction |
|
 Minimal Invasive Surgery, Minimal Incision Surgery, or Pericutaneous Surgery, permits surgery in the affected area performed with a small incision.
Minimal Invasive Surgery, Minimal Incision Surgery, or Pericutaneous Surgery, permits surgery in the affected area performed with a small incision.
MIS of the foot respects the joint surfaces, does not use ischemia and in general internal fixation is not required. The same pre operative indications and studies are performed as in traditional surgery, (Dr. Mariano De Prado).
Comparable results are obtained as those in traditional surgery with less pain and shorter incapacity.
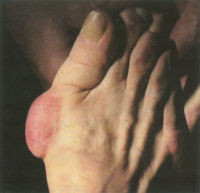
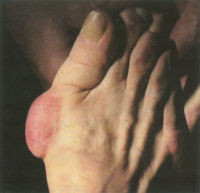
One problem that confronts the surgeon when attending a patient with hallux valgus, as with any orthopedic pathology that we treat surgically, is to make the adequate decision of what procedure to use to get the best treatment or combination of treatments.
When confronted with a patient with hallux valgus many questions arise. Should we just do an exostectomy, or should we do a distal metatarsal osteotomy, or proximal, or just soft tissue corrections. In the end, we have a complicated problem that has resulted in more than 200 surgical procedures reported which we can use to treat this pathology.
The most important part of forefoot surgery as in all orthopedic surgery is the indications and that the techniques that we select are correct and to perform a procedure or technique that we dominate and are familiar with but more important it must be indicated to resolve the problem of hallux valgus. (Dr. Ramon Viladot) It is obvious that we would not use the same procedure or series of procedures for a patient that has a mild or severe bunion, patient is young or old, if the intermetatarsal angle is normal or larger than 20 degrees or if they have a normal or abnormal PASA and DASA.
 The distal articular angle of the 1st metatarsal phalangeal joint named PASA (proximal articular set angle), or DMAA (distal metatarsal articular angle), is normal between 0 and 8 degrees. This factor with the intermetatarsal angle and DASA angle with the age of the patient, their activities or parts of the deformities of hallux valgus that lead us in the direction to select the proper protocol or techniques in the correction of hallux valgus.
The distal articular angle of the 1st metatarsal phalangeal joint named PASA (proximal articular set angle), or DMAA (distal metatarsal articular angle), is normal between 0 and 8 degrees. This factor with the intermetatarsal angle and DASA angle with the age of the patient, their activities or parts of the deformities of hallux valgus that lead us in the direction to select the proper protocol or techniques in the correction of hallux valgus.
MIS surgical techniques is a good valid alternative in forefoot surgery. Always the indications must be correct and the surgeon must have a good preparation and use the proper instrumentation and material needed to perform this type of surgery. (Dr. Ramon Viladot). Following the principles of Minimal Invasive Surgery we can perform the following procedures or surgical acts:
|
| |
Exostosis (Modified Silver) |
|
Osteotomies in the 1st metatarsal can be distal metatarsal osteotomy such as the ReverdinIsham with a medial wedge respecting the lateral cortex and performing an Osteoclasis to correct the PASA and we can also perform a modification of this osteotomy by completing it and sliding the metatarsal head laterally thereby increasing the relative closure of the 1st intermetatarsal angle. Next we can do a proximal metatarsal osteotomy performed with a wedge osteotomy proximal laterally to close the intermetatarsal angle. Another procedure that we can perform is an abductor release which is a Modified McBride. The next procedure we can do is also an osteotomy of the base of the proximal phalanx (Akin).
The combination of one or more of these procedures or surgical acts depends upon the type of patient, the severity of the deformity, these procedures can take us to the correction of the vast majority of the patients who suffer in hallux valgus. When evaluating your patients with hallux valgus, and deciding which procedures or surgical acts, the following is important to aide in your decision process.
- The age of the patient
- The activity
- By radiographic examination we can determine the PASA angle, the intermetatarsal angle, the DASA angle using the following protocol we will be able to correct the majority of hallux valgus deformities
|
| |
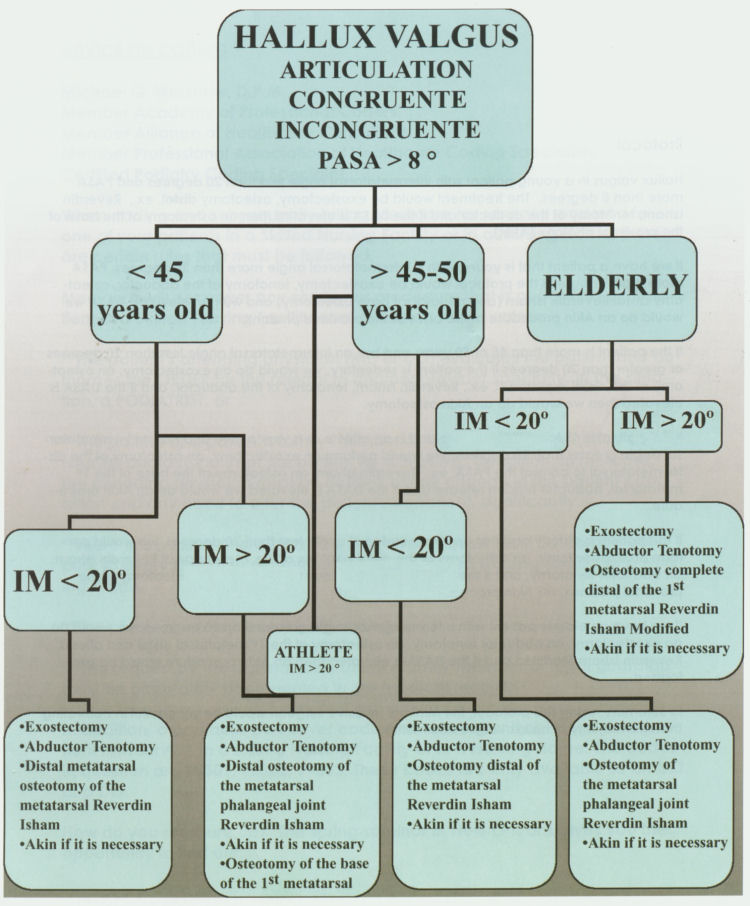
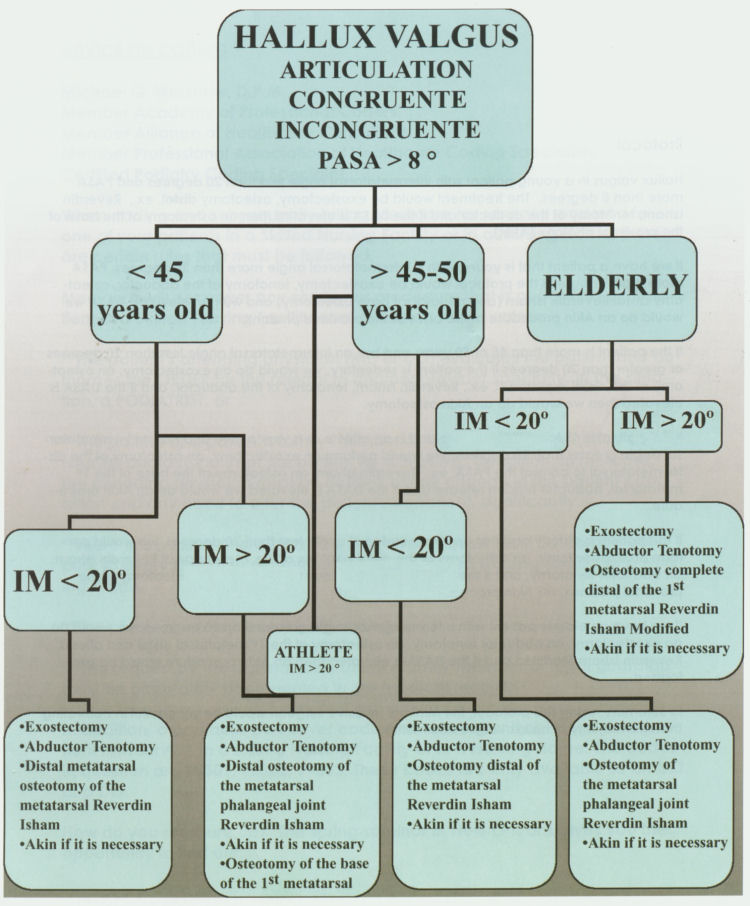
Protocol |
|
Hallux valgus in a young patient with intermetatarsal angle less than 20 degrees and PASA more than 8 degrees. The treatment would be exostectomy, osteotomy distal, ex., Reverdin Isham, tenotomy of the abductor and if the DASA is elevated then an osteotomy at the base of the proximal phalanx (Akin).
If we have a patient that is young with a intermetatarsal angle more than 20 degrees, PASA more than 8 degrees the protocol would be exostectomy, tenotomy of the abductor, osteotomy distal Reverdin Isham (and metatarsal base osteotomy) and with an elevated DASA we would do an Akin procedure at the base of the proximal phalanx.
If the patient is more than 45 or 50 years and has an intermetatarsal angle less than 20 degrees or greater than 20 degrees if the patient is sedentary, we would do an exostectomy, an osteotomy of the distal metatarsal, ex., Reverdin Isham, tenotomy of the abductor, and if the DASA is elevated then we would do an Akin osteotomy.
If the patient is 45 to 50 years of age and is an athlete or is very active and has an intermetatarsal angle greater than 20 degrees, we would perform an exostectomy, an osteotomy of the distal metatarsal to correct the PASA, ex., Reverdin Isham, an osteotomy at the base of the 1st metatarsal, abductor tendon release and if the DASA is elevated we would do an Akin procedure.
If the patient is elderly and has an intermetatarsal angle less than 20 degrees, we would perform an exostectomy, an osteotomy of the distal phalanx of the 1st metatarsal Reverdin Isham, an abductor tenotomy, and if the DASA is elevated then we would do an osteotomy of the proximal phalanx, an Akin procedure.
If we have an elderly patient with intermetatarsal angle greater than 20 degrees, we would do an exostectomy, an abductor tenotomy, an osteotomy of the 1st metatarsal distal and after a Reverdin Isham Modified and if the DASA is elevated then an Akin procedure would be performed.
In summary, using this protocol, the Minimal Invasive surgeon would be successful in correcting the vast majority of hallux valgus deformities.
|
| |
Flowchart |
|
Click on the flowchart to view full size.
|
| |
Bibliography |
- Anderson R. MD: American Academy of Orthopaedic Surgeons: Reconstrucción de tobillo y pie. OKU 6, Capítol 12, 257-280, 2001
- Austin, D. And Leventen. E.A new astronomy for hallux valgus. Clin Orthop 157: 25-30, 1981.
- Coughiin, M.J.: Chevron procedure. Contemp Orthop, 23; 45-49, 1991
- Del Prado, Mariano: El tratamiento quirúrgico percútaneo del hallux valgus. Tesis doctoral, 1997-1998 España.
- De Prado: Cirugía Percutanea del pie, técnicas quirúrgicas indicaciones bases anatómicas; Masson, 2003, España.
- Hattrup, S. and Johnson K. Chevron Astronomy; Analysis of Factors in patients dissatisfaction. Foot and ankle, 5: 327-332, 1985
- Isham: Isham minimal invasive, percutaneous procedures for correction of lesser digital deformities
- Johnson K., Cofield R. and Morrey, B. Chevron astronomy for hallux Valgus. Clin Orthop 142; 44-47, 1979.
- Kelikian. McGraw-Hill Interamericana; México 2001; Translated from thefirstEnglish edition of Operative Treatment of the foot and Ankle, By Armen Kelikian 1999.
- Leventen, E: The Chevron procedure. Orthopedics, 13: 973-978, 1990
- Mascaro R.: Patología de los dedos: diez lecciones sobre patología del pie, A. Viladot, 185- 209, 1979
- Mizel M. MD: American Academy of Orthopaedic Surgeons: Deformities ofthe lesser toes and metatarsophalangeal joint disorders, OKU foot and ankle 2, Chapter 13, 163-173, 1998.
- Mizel M; Sobel M., Ptaszek AJ: Disorders of the foot and ankle, Review of orthopaedics Miller, cap 5,279-303, Ed Saunders 2000.
- The Academy of Ambulatory Foot & Ankle Surgery; Preferrend Practice Guidelines. Hallux abductovalgus
- Viladot Ramón: Rev Ortop Traumatol 2002; 46(6);487-489
|
| |
Contact |
Dr. R. Esteban Galaz L.
Av. Tamaulipas 601, Centro; CP 89000, Tampico Tams
(52) 78-38-34-36-17
(52) 78-38-34-50-70
(52) 83-32-12-62-01
draalaz@prodiav.net.mx
|
|
|
|

 Minimal Invasive Surgery, Minimal Incision Surgery, or Pericutaneous Surgery, permits surgery in the affected area performed with a small incision.
Minimal Invasive Surgery, Minimal Incision Surgery, or Pericutaneous Surgery, permits surgery in the affected area performed with a small incision.
 The distal articular angle of the 1st metatarsal phalangeal joint named PASA (proximal articular set angle), or DMAA (distal metatarsal articular angle), is normal between 0 and 8 degrees. This factor with the intermetatarsal angle and DASA angle with the age of the patient, their activities or parts of the deformities of hallux valgus that lead us in the direction to select the proper protocol or techniques in the correction of hallux valgus.
The distal articular angle of the 1st metatarsal phalangeal joint named PASA (proximal articular set angle), or DMAA (distal metatarsal articular angle), is normal between 0 and 8 degrees. This factor with the intermetatarsal angle and DASA angle with the age of the patient, their activities or parts of the deformities of hallux valgus that lead us in the direction to select the proper protocol or techniques in the correction of hallux valgus.