| |
The Isham Bunionette Procedure for the Correction of Moderate to Severe Tailor's Bunion Deformities
A Double Osteotomy Metatarsal Procedure
Author: Dr. Stephen A. Isham
|
Introduction |
|
The surgical procedures presented are for the treatment of moderate to severe Tailor's bunion deformities by performing an abductory wedge osteotomy in the metaphyseal area of the 5th metatarsal head at an angle, preserving the articular surface of the 5th metatarsal phalangeal joint, and an adductory wedge osteotomy in the mid-shaft or base of the 5th metatarsal, resulting in the correction of the structural deformity. The Isham Bunionette procedure with its pre-operative criteria, techniques of operation, post-operative management, advantages, and disadvantages are presented.
|
| |
Definition |
Tailor's bunion deformity is a combination of a transverse and frontal plane deformity of the 5th digit on the 5th metatarsal phalangeal head. In this deformity the 5th digit is medially rotated toward the lesser digits, and rotated with its dorsal surface more laterally. Most bunionette deformities, mild, moderate, or severe, contain some combination of these deformities. These deformities contain both soft tissue and osseous components called positional and structural deformities.
|
| |
Etiology |
|
The primary cause of bunionette or tailor's bunion deformities is the abnormal foot structure which, as dictated by genetic code, is exposed to abnormal pronatory forces resulting in hypermobility of the osseous structure and an over dependence on soft tissue structures for stability during weight-bearing. In particular during the last phase of the propulsive stage of gait. The severity of the bunionette deformity is proportionate to the severity of the abnormal pronatory forces present.
Other causes of bunionette deformities are systemic diseases, such as gout or rheumatoid arthritis, neurological disorders and trauma causing permanent osseous or soft tissue damage to the 5th ray.
Footwear, although not a primary cause can aggravate the symptoms of the deformity.
|
| |
Classification |
|
The classification of deformities is an instrument that enables the podiatric surgeon to select or modify a procedure to achieve its best results for each patient. It is important that we realize that surgery is an art, and we must treat the patient as a whole and not as a set of radiographs and collection of angles and measurements. To classify the severity of a bunionette deformity, the following measurements are commonly used by the author: proximal articular set angle, 4th intermetatarsal angle, lateral deviation angle, and 5th metatarsal phalangeal joint position.
Proximal Articular Set Angle of the 5th MPJ
The proximal articular set angle of the 5th MPJ is formed by the bisection of the longitudinal axis of the 5th metatarsal and the active cartilage of the head of the 5th metatarsal.
4th Metatarsal Angle
The 4th intermetatarsal angle is formed by the bisection of the line of the longitudinal axis of the 5th and 4th metatarsals. Lower range is between 6 and 8 degrees.
Lateral Deviation Angle
The lateral deviation angle is a measurement of the lateral bowing of the 5th metatarsal, involving the distal and middle portions of the 5th metatarsal bone. Figure 1. Normal range under 7 degrees.
5th Metatarsak Phalangeal Joint Position
5th metatarsal phalangeal joint position (MPJ) has 3 components:
- Congruous - The articular surface of the 5th MPJ is parallel or equal.
- Deviated - The articular surface of the 5th MPJ is unequal. The lines of the intersection fall outside the joint.
- Subluxed - The articular surface of the 5th MPJ is unequal with the lines intersecting inside the MPJ.
The presence of a deviated or subluxed joint position is evidence of the presence of increased positional deformity.
|
|
| |
Classification of Tailor's Bunionette Deformity |
|
The classification of tailor's bunion deformities is divided into 3 classifications: mild, moderate and severe.
Mild Bunionette Deformity
This deformity has an intermetatarsal angle of 6 to 8 degrees and the joint surface is generally congruous.
Moderate Bunionette Deformity
Moderate bunionette deformities have an intermetatarsal angle between 8 and 11 degrees. In moderate tailor's bunion deformities the 5th MPJ position is generally deviated.
Severe Bunionette Deformity
The deformities of severe tailor's bunionettes contain an intermetatarsal angle of 12 degrees or greater and generally the joint position is subluxed.
|
| |
Isham Bunionette Procedure |
|
The author, recognizing the similarities in function and deformity of the 1st and 5th rays, developed a new procedure for the correction of bunionette deformities, based on the highly successful Reverdin-Isham bunionectomy procedure for the correction of hallux abducto valgus.
An increased proximal articular set angle in the bunionette deformity, as with the HAV deformity, results in instability of the MPJ, and increased structural and positional forces that increase the 4th intermetatarsal angle.
The author, using the Isham osteotomy, performed this lateral wedge osteotomy in the head of the 5th metatarsal at an angle from dorsal distal, just proximal to the articular surface on the dorsal aspect of the head, to plantar proximal, at a point just proximal to the articular surface on the plantar aspect of the 5th metatarsal head. This placement of the Isham osteotomy preserves and repositions the articular surface and corrects the proximal articular set angle, and redirects and stabilizes the forces at the 5th metatarsal phalangeal joint. The placement of the osteotomy inside the joint capsule in the cancellous bone of the 5th metatarsal head, proved to be highly stable and eliminated the need for internal fixation. A second osteotomy on the same plane, dorsal distal to plantar proximal, was performed creating a medial wedge osteotomy at the area of the deformity in the shaft or base of the 5th metatarsal, correcting the lateral deviation angle, and the 4th intermetatarsal angle (Fig. 2). As hoped, the post-operative management proved to be the same as needed for a single osteotomy procedure. No increased pain or disability was noted and marked improvement of the short and long term results was immediately apparent.
|
|
|
| |
Preoperative Criteria |
|
This procedure is directed at the structural correction of tailor's bunion deformities that are manifested at the metatarsal head and at the shaft of the 5th metatarsal. Specific criteria for the Isham bunionette procedure are:
- A symptomatic bunionette deformity.
- Good range of motion of the 5th MPJ; no pain, no crepitus, and no degenerative changes.
- A congruous, deviated or subluxed joint.
- An intermetatarsal angle of over 8 degrees.
- A lateral deviation angle of over 7 degrees.
- An increased PASA.
A plantarflexed 5th metatarsal may or may not be present. Another procedure to correct the plantarflexed metatarsal is not needed.
|

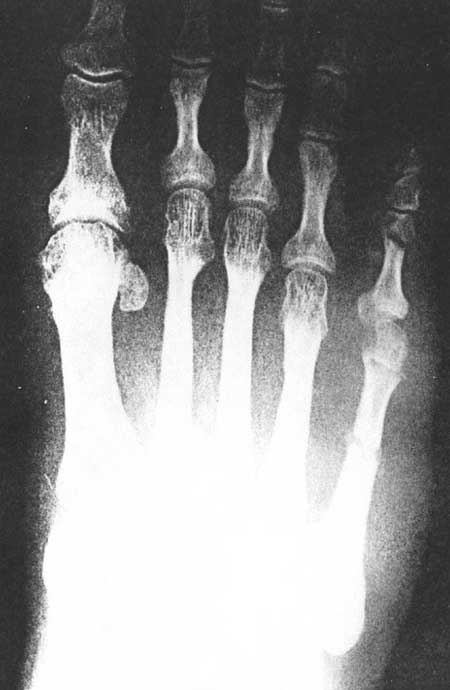
Fig 3A. (pre-operative)
|
|

Fig 3A (post-operative)
|
| |

Fig 3B (pre-operative)
|
|

Fig 3B (post-operative)
|
| |

Fig 3C (pre-operative)
|
|
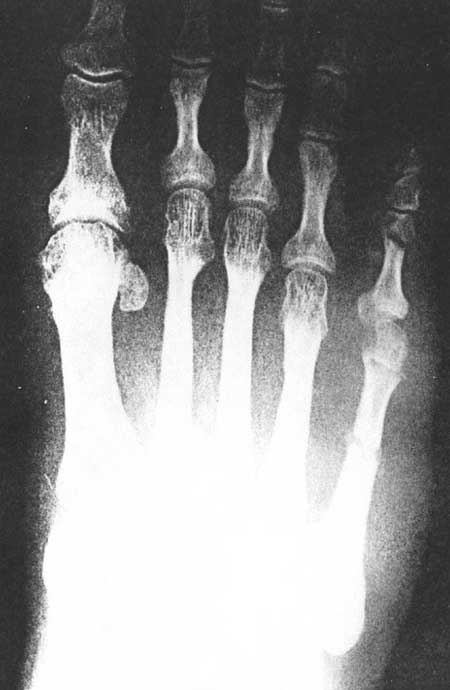
Fig 3C (post-operative)
|
|
| |
Operative Techniques |
|
The Isham Bunionette Procedure is performed using one of two surgical techniques; a minimal incision technique, and an open exposure technique.
Minimal Incision Technique
A 0.25 cm incision is made over the head of the 5th metatarsal, just lateral to the extensor tendon. The incision is then deepened, underscored and retracted exposing the joint capsule. A similar incision is made through the joint capsule, through which the hypertrophied aspect of the 5th metatarsal head is excised, and a lateral wedge osteotomy is performed from dorsal distal to plantar-proximal, correcting the medial deviation of the 5th metatarsal head and placing the 5th digit in an improved position. A second 0.25 cm incision is made over the shaft of the 5th metatarsal, lateral to the extensor tendon, approximately 2.0 cm proximal from the first incision. The second incision is deepened, underscored and retracted exposing the shaft of the 5th metatarsal and a medial wedge osteotomy is performed, correcting the splaying of the 5th metatarsal (Fig. 3). The wound is dressed and the position is maintained with a sterile splint dressing of the surgeon's choice.
Post-operative Management
Patient is given a post-operative shoe and is discharged. The patient is allowed to increase ambulation to tolerance. Post-operative pain, as with most ambulatory procedures, requires a minimal amount of pain control medications. Many patients take none.
The dressing is changed on the second or third day after surgery and the sutures are removed. A splint dressing is applied. The second dressing change occurs ten days post-operatively. This removable splint dressing is applied and changed daily by the patient. Bathing is permitted. The patient is allowed to ambulate in a self-surgical shoe or a supportive athletic type shoe until normal shoes can be worn. Post-operative radiographs are taken at the first dressing change and then again three to four weeks after surgery to evaluate the healing. It should be noted that, as with a Reverdin-Isham bunionectomy, a minimal amount of bony callous formation is noted at the distal osteotomy site. However, more is noted at the proximal osteotomy site.
Open Exposure Technique
A 5.0 longitudinal incision is made over the dorsal aspect of the 5th MPJ, lateral to the extensor apparatus. The incision is deepened through the subcutaneous tissues exposing the joint capsule, and a capsulotomy is performed. The head is freed of the capsule ligaments and attachments. The head of the 5th metatarsal is delivered through incision and the lateral eminence is then resected. An angular lateral wedge osteotomy is performed using a bone cutting instrument of the surgeon's choice. The angulation is formed dorsal distal, at the termination of the cartilage on the dorsum of the head, to plantar proximal at the termination of the cartilage of the plantar surface of the metatarsal head. The medial cortex is left intact. The osteotomy site is closed correcting the deformity on two planes. Internal fixation is a prerogative of the surgeon. The capsule is closed using 2-0 absorbable sutures. A second osteotomy is performed either mid-shaft, for moderate deformities, to base, for severe deformities on the same plane. However, this osteotomy is a medial wedge osteotomy closing the 4th intermetatarsal angle. The lateral cortex is left intact. Internal fixation is a prerogative of the surgeon. The skin is sutured with 4-0 nylon closure.
Post-operative Management for Technique B
Post-operative care for open techniques is the same for minimal incision techniques, except for one exception. The foot is kept in a post-operative shoe for 3 to 4 weeks. It is my opinion that the open technique requires more soft tissue dissection, resulting in increased instability at the osteotomy site. This increased instability indicates longer use of a post-operative shoe. Ambulatory osteotomy fixation techniques and immobilization is at the discretion of the surgeon.
|
| |
Post Operative Bandaging |
|
Minimal incision procedures by design are very atraumatic, with a minimal amount of soft tissue disruption. A second metatarsal, for example, has 7 tendons passing over the MPJ. These tendons pass over the dorsal, medial, plantar, and lateral aspects of the MPJ. The head of the second metatarsal is also stabilized by a strong intermetatarsal ligament attached to the 3rd, 4th, and 5th metatarsals. A properly performed osteotomy at the proximal aspect of the head does not disrupt these soft tissues, nor does the proximal osteotomy. These structures, during the initial post-operative healing phase, the first 3 to 6 weeks, contract and stabilize the osteotomy site. This contracture of the soft tissue structures is called "intrinsic fixation". Although internal fixation is not required, external splinting is required to enable the patient to bear weight.
Post-operative splint dressings in minimal incision surgery should stabilize the surgical site in its corrected position, be a comfort to the patient, be easy to apply, and maintain a sterile barrier.
My post-operative dressings are presented in two phases. The first phase represents the type of dressing used during the first post-operative week. These dressings are applied by the surgeon. The second phase of dressings are those splint dressings used the following four weeks. Figure 4 represents phase one dressings, and Figure 5 represents phase two dressings. The phase two dressings are initially applied by the surgeon and are changed daily by the patient, after they have been instructed in application. Bathing is permitted on a daily basis, after the first post-operative week.

Fig 4A. Intraoperative Dressings
|
|

Fig 4B. Intraoperative Dressings
|
| |

Fig 4C. Intraoperative Dressings
|
|

Fig 4D. Intraoperative Dressings
|
| |

Fig 5. Bandaid Wound Cover
|
|

Fig 5. Coban Splint
|
|
| |
Advantages of The Isham Bunionette Procedure |
- It provides biplane correction of the structural deformity with improved position of metatarsals.
- It corrects the PASA angle of the 5th metatarsal.
- It involves minimal amount of post-operative disabilities, similar to a simple osteotomy procedure.
- It can be performed in the presence of uncontrollable pronatory forces.
|
| |
Disadvantages of The Isham Bunionette Procedure |
- If poor healing takes place at the osteotomy site, possible shortening of the metatarsal may occur.
- It cannot be performed on children prior to epiphyseal closure.
|
| |
Summary |
|
The Isham Bunionette procedure, as presented, is an excellent procedure for the correction of moderate to severe tailor's bunion deformities that can correspond to the pre-operative criteria outlined. It should prove to be highly effective to both the ambulatory and hospital based surgeons alike.
|
| |
References |
- Akin, O.F.: "The Treatment of Hallux Valgus: A New Operative Procedure and Its Results." Medical Sentinel. 1925.
- Campbell, D.C.: "Chrevron Osteotomy for Bunionette Deformity," (abstract). Foot and Ankle. 1982.
- Colloff, B., Weitz, E.N.: "Proximal Phalangeal Osteotomy and Hallux Valgus." Clin. Orthop. 1967.
- Diebold, P.F.: "Basal Osteotomy of the Fifth Metatarsal for Bunionette." Foot and Ankle. 1991.
- DuVries, H.L..: "Surgery of the Foot," The C.V. Mosby Co., St. Louis. 1965.
- DuVries, H.L.: "Surgery of the Foot" 4th Ed. C.V. Mosby, St. Louis. 1978.
- Fallat, L.M., Bucholz, J.: "Analysis of Tailor's Bunions by Radiographic and Anatomical Display." J. American Podiatry Assoc. 1980.
- Funk, J.F., Wells, R.: Bunionectomy With Distal Osteotomy." Clin. Orthop. Rel. Res. June 1972.
- Gerbert, J." "Textbook of Bunion Surgery." Mount Kisco, New York, Futura Publishing Co. 1981.
- Gerbert, J., Melillo, T.: "A Modified Akin Procedure for the Correction of Hallux Valgus." Journal Amer. Podiatr. Assoc. 1971.
- Gerbert, J., Mercado, O.A., Sokoloff, T.H.: "The Surgical Treatment of Hallux Abducto Valgus and Allied Deformities." In: Podiatric Med. And Surg.: Monograph Series." Mount Kisco, New York, Futura Publishing Co. 1973.
- Gerbert, J., Sgarlato, T.E., Subotnick, S.I.: "Preliminary Study of a Closing Wedge Osteotomy of the Fifth Metatarsal for Correction of a Tailor's Bunion Deformity." J. Am. Podiatry Assoc. 1972.
- Gray, H.: "Grays Anatomy, 36th Ed." W.B. Saunders, Philadelphia. 1980.
- Isham, S.A.: "The Reverdin-Isham Procedure for the Correction of Hallux Abducto Valgus." Current Podiatr. Med. 1985.
- Isham, S.A.: "Reverdin-Isham Procedure for the Correction of Hallux Abducto Valgus." Clinics in Podiatric Medicine and Surgery-Vol. 8, No. 1. January 1991.
- Kaplan, E.G., Kaplan, G., Jacobs, A.M.: "Management of Fifth Metatarsal Head Lesions by Biplane Osteotomy." J. Foot Surg. 1976.
- Keating, S.F., DeVincentis, A., Goller, W.L.: "Oblique Fifth Metatarsal Osteotomy: A Follow Up Study." J. Foot Surg. 1982.
- Kelikian, H.: "Hallux Valgus, Allied Deformities of the Forefoot and Metatarsalgia." W.B. Saunders Company, Philadelphia, Pennsylvania. 1965.
- Konradsen, L., Nielsen, P.T.: "Distal Metatarsal Osteotomy for Bunionette Deformity." J. Foot Surg. 1988.
- Leach, R. E., Igou, R.: "Metatarsal Osteotomy for Bunionette Deformity." Clin. Orthop. 1974
- Mercado, O.A.: "An Atlas of Foot Surgery." Vol. 1. Carolando Press, Oak Park, Illinois. 1979.
- Peabody, C.W.: "Surgical Cure of Hallux Valgus." Journ. Bone Joint Surg., Vol. 13A. 1931.
- Podiatrics Sino-American Conference On Foot Disorders, Beijing, CHINA, October, 1987.
- Pritt, Donald S.: "Documentation of Successful Non-Fixation of Osteotomies in 700 Cases." Journal: Current Podiatry. July, 1980.
- Root, M.L., Orien, W.P., Weed, J.H.: "Normal and Abnormal Function of the Foot." Vol. 2. L.A. Clinical Biomechanics Corp. 1977.
- Rosen, Stanford: "Closing Dorsal Wedge Osteotomy." Journal: The Journal of the AAFS. Vol. 2. 1984.
- Sakoff, M., Levy, A.I., Hanft, J.R.: "Metaphyseal Osteotomy for the Treatment of Tailor's Bunions." J. Foot Surg. 1989.
- Sgarlato, T.E.: "Compendium of Podiatric Bio-mechanics." California College of Podiatric Medicine, San Francisco. 1971.
- Sponsel, K.H.: "Bunionette Correction by Metatarsal Osteotomy: Preliminary Report." Orthop.-Clin.-North-Am. 1976.
- Stauffer, Richard N., M.D.: "Orthopedic Surgery." J. of the Am. Med. Assoc., Vol. 252. October 26, 1984.
- Steinke, M.S., Boll, K.L.: "Hohman-Thomasen Metatarsal Osteotomy for Tailor's Bunion (Bunionette)." J. Bone Joint Surg. 1989.
- Strauss, Ronald J.: "Lesser Metatarsals and Hammertoes." Journal: Current Podiatry, January, 1982.
- Wilner, Ronald J.: "Osteoclasis, A Discussion." Journal: JAPA Vol. 63, No. 1, January, 1973.
- Winquist, Robert A.: "Closed Intramedullary Osteotomies of the Femur." Journal: Clinical Orthopedics and Related Research. August 30, 1985.
- Wood, William A.: "Fixation Versus Non-Fixation of Osteotomies of the Foot." Journal: JAPMA. Vol. 76. April, 1986.
- Wu, K.: "Surgery of the Foot." Lea & Febiger, Philadelphia. 1986.
- Yancey, H.A.: "Congenital Lateral Bowing of the Fifth Metatarsal." Clin. Orthop. 1969.
|
|
|
|